- Location: Chillicothe, OH
- Number of Beds: 311
- Number of Employees: 2500
- Founded: 1895
- HIS System: MEDITECH
The Challenge
Drew Hinty, Coordinator, Payer Relations & Contracting, is part of a department of six – which also includes an analyst, specialist, director, and two provider enrollees. Adena uses MEDITECH as its core HIS system for hospital facilities and eClinicalWorks (ECW) for its physicians.
Several years ago, the Department found itself in transition following staff turnover. Drew and others new to the department were faced with learning about their new systems and processes as they went along. One particular challenge beyond their control was the evolution of third-party payer contracts.
As third-party payers shift from a “fee-for-service” or “percent of charge” reimbursement model to value-based reimbursement, contract terms, coding, and their interpretations inevitably become more complex.
Adena’s third-party contracts are undergoing a shift toward the following:
- Value-based contracts: A reimbursement model in which a portion of the provider’s payment is tied to performance, based on cost efficiency and quality performance measures.
- DRG (Diagnosis Related Group) Reimbursement Methodology: A methodology that pays the provider, based on the weight assigned to the DRG code that is used to adjust for the fact that different types of patients consume different resources and therefore have different costs. Weights are updated annually by Centers for Medicaid and Medicare Services (CMS) to reflect changes in medical practice patterns, use of hospital resources, diagnostic and procedural definitions and MS-DRG assignment criteria.
- HEDIS (The Healthcare Effectiveness Data and Information Set): An incentive-based reimbursement model that measures performance based on care and service. Established by the NCQA (National Committee for Quality Assurance), HEDIS consists of 71 measures across 8 domains of care. According to NCQA, this is used by more than 90% of America’s health plans to measure performance on important dimensions of care and service.
This new reality, coupled with the fact that Adena Health contracts with 32 different payers, causes projections to be nearly impossible when calculated manually. “We previously used tools like Microsoft Access and Microsoft Excel, but there are simply too many variables and too much data involved to try and project future reimbursements,” explained Drew. “If contracts are not the same as they were previously, you cannot use the same tools.”
The Solution
During the vendor selection process, Adena searched for a solution that could accurately calculate reimbursements and identify opportunities for collecting underpayments. After a thorough investigation process, Adena chose PMMC because of its strong reputation through word-of-mouth and referrals based on results and its high level of customer service. Adena implemented PMMC CONTRACT PRO in 2008 to manage its third-party payer contracts, and to help identify underpayments. Adena’s Revenue Cycle Department has a 2014 goal to collect $450,000 in underpayments. In 2013, Adena implemented PMMC ESTIMATOR PRO to generate patient estimates based on the claim data from CONTRACT PRO.
Drew and his department chose to strategically focus on simulating future proposed contract terms with their top five payers. In May 2014, Adena “turned on” the SIMULATOR function of CONTRACT PRO when it was time to re-negotiate with one of their largest payers. The tool played a huge role in managing the data and using it to report internally.
“Contract PRO SIMULATOR is the only tool I was going to use,” he said.
The Results
The findings provided from CONTRACT PRO SIMULATOR were dramatic.
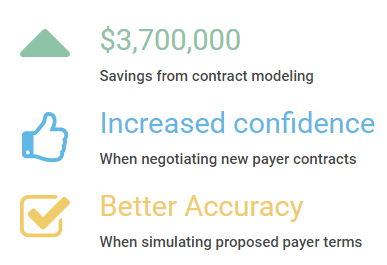
After plugging in the proposed contract terms, Adena realized it would have lost $3.7 million in reimbursement dollars had it just agreed on the terms without modeling them.
Because the tool pulls EDI 835 and EDI 837 claim data, Drew had the accurate data he needed when entering negotiations. “I could have never done this without CONTRACT PRO SIMULATOR. There are simply too many variables involved,” explained Drew. Not only did the savings have an obvious financial impact, it boosted the morale and confidence among the staff that the department was headed in the right direction.
“This allows us to go into new negotiations with the utmost confidence,” added Drew.
As Adena continues to move away from percent of charge and toward value-based contracting, it will be using CONTRACT PRO SIMULATOR exclusively, including with two more of their payers for their evergreen contracts. “This is the ‘be-all and end-all’ of how we will analyze and manage rates,” Drew concluded. “This is the only system that can give us the future state.”
Learn more about contract modeling and hospital contract management.